by Stephen F. Jencks, M.D., M.P.H.
[Also see companion post by Joanne Lynn, M.D.]
Issue.
The Medicare Readmission Reduction Program (MRRP) encourages hospitals to reduce readmissions within 30 days of discharge by imposing substantial financial penalties on hospitals with more readmissions than would be expected if the same patients were discharged from an average hospital.[1] But some hospitals and communities have succeeded too well and reduced discharges even more than readmissions so that their readmission rates, as currently calculated, do not improve much, which puts them at higher risk for penalties. There are two underlying problems:
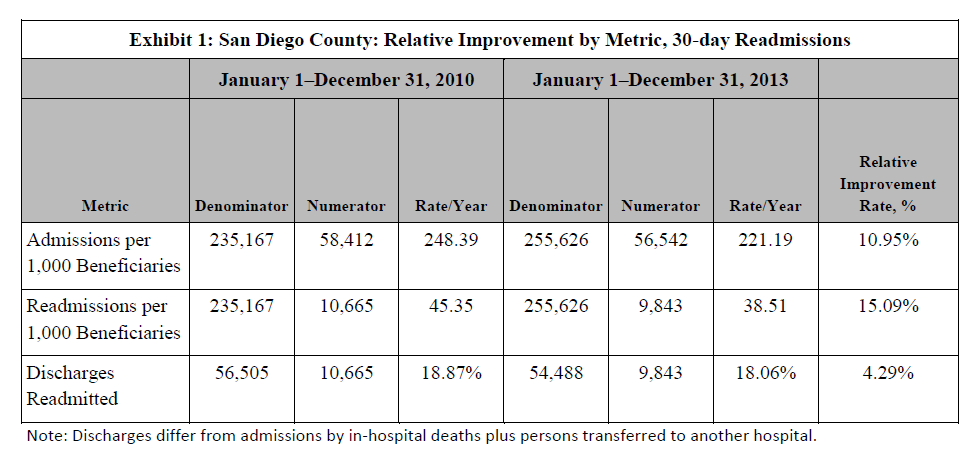
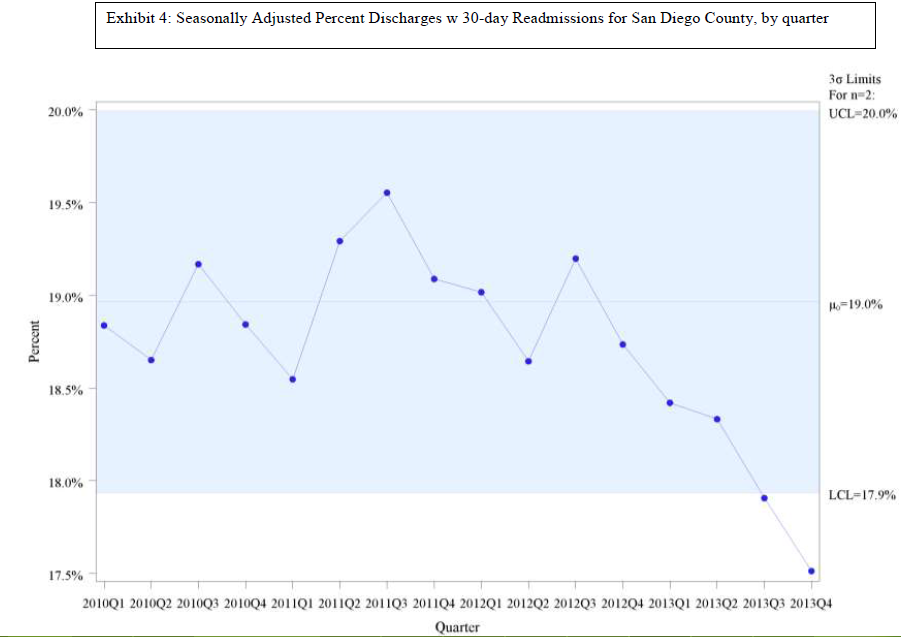
First, there are two ways of thinking about, and therefore measuring, the rate of readmissions; and they often lead to quite different results and quite different decisions on penalties. One is discharge-based; the other, population-based. The relationship between the two is simple: (readmissions/discharges) X (discharges/(beneficiary population (1,000s) ) ) = readmissions / (beneficiary population (1,000s))
Patients who are admitted but die during hospitalization or are transferred to another hospital are not counted as discharges from the first hospital.
Second, effective interventions to reduce 30-day readmissions have an effect on admissions that extends far beyond 30-days after discharge and they reduce a lot of other admissions, especially if implemented in partnership with community providers and services.
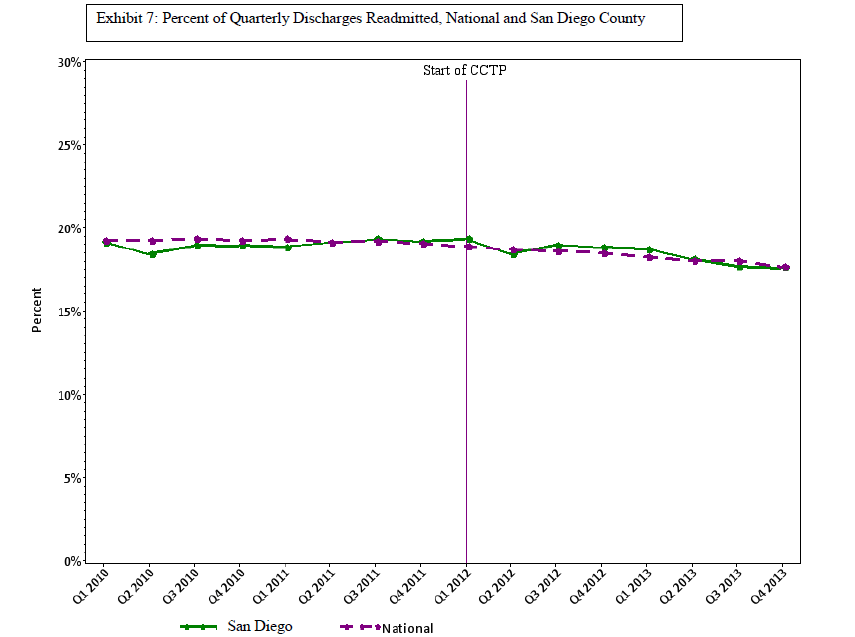
When Congress created the MRRP, many stakeholders had become aware (and dismayed) that 20% of people enrolled in Medicare fee-for-service and discharged from a hospital were readmitted within 30 days of hospital discharge. Clinical trials had shown that improved processes around hospital discharges could prevent many of these readmissions. The aim of establishing accountability also made a hospital focus desirable. In this view, readmission is a burden resulting from poor hospital discharge processes, whether clinically premature or poorly executed. With that emphasis on discharge processes as cause and cure for readmissions, it was natural for the Centers for Medicare & Medicaid Services (CMS) to choose to estimate each hospital’s expected readmissions as the number of patients whom the hospital discharged and who would be expected to be readmitted after discharge from an average hospital. Most readmission reduction initiatives use this discharge-based readmission rate to measure performance. This discharge-based perspective effectively defines the readmission rate as the percentage of discharges that are followed by a readmission. In this way of thinking, the number of hospital discharges is simply a fact of life, much like the fact that a year has 365.24 days. This view does not see that hospital actions might reduce the number of patients they discharge, and this blind spot causes trouble.
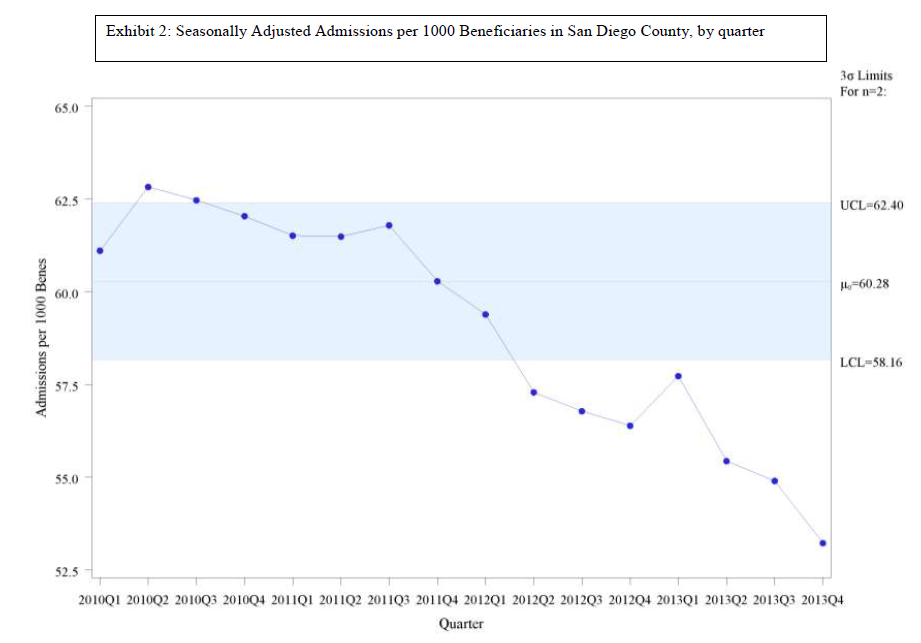
Hospitals actually have a great deal of influence on how many patients they admit and discharge because so many of their discharges are admitted through their emergency department or by hospital-affiliated physicians and because they can collaborate with community services and providers who can forestall patients even coming to the hospital. Population-based hospital discharge rates vary substantially across regions, and they can change over time.
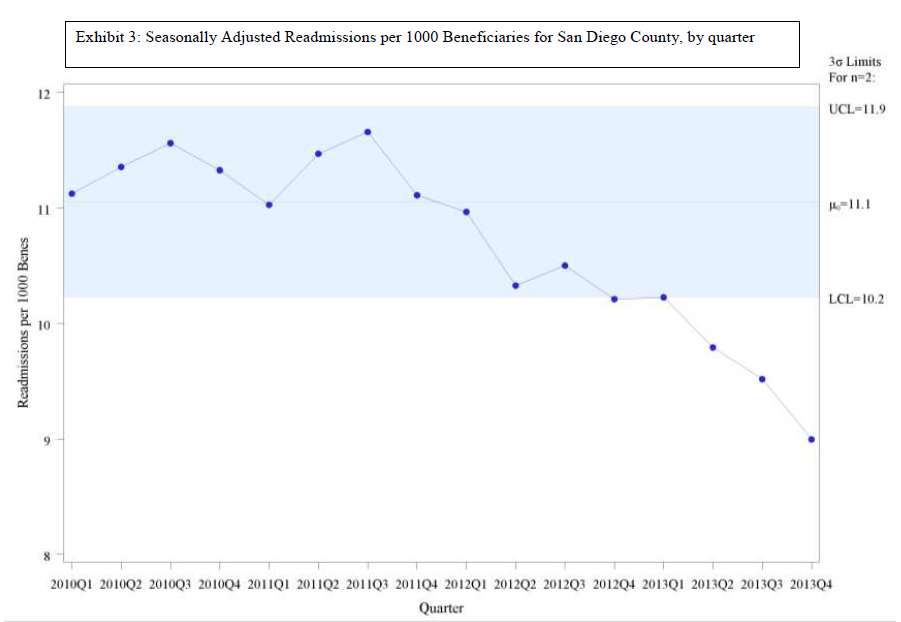
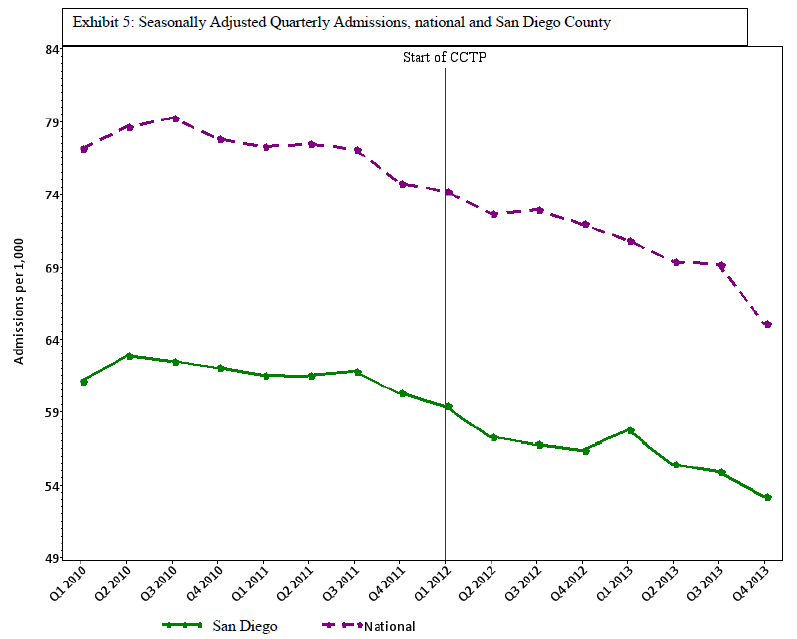
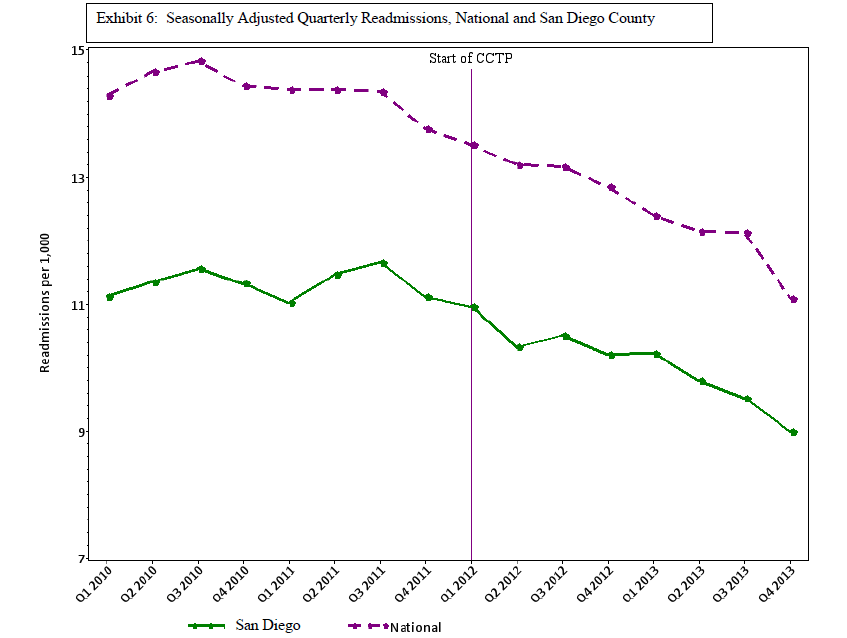
Some policy makers worried that the discharge-based rate could behave in unexpected ways if hospitals took steps that reduced total discharges by more than the reduction in 30-day readmissions. As a result, several programs, such as the Partnership for Patients and the Quality Improvement Organizations’ (QIOs) Care Transitions Program, were designed using a population-based readmission rate or converted to such a rate after evaluating early findings. The population-based rate is the number of readmissions for every 1,000 fee-for-service Medicare beneficiaries in the hospital’s service area. This view sees readmissions as a community health problem, a burden on a population of beneficiaries and the Medicare trust funds that is associated with that population’s use of hospitals just as hospital-acquired infections are associated with use of hospitals. From this perspective, preventing hospitalizations, improving discharge transitions, and improving post-discharge care are equally valid ways to reduce readmissions. Whether the hospital reduced hospitalizations in order to reduce readmissions is less important than being sure that we do not penalize hospitals for taking such steps. Population-based rates are closely aligned with the three-part aim of the National Quality Strategy (individual care, population health, and affordability), not only because they are population-based but also because they reflect the close relationship between care in the community and a hospital’s apparent performance.
Thus, a program can reduce burdens on beneficiaries and Medicare through significant reductions in the population-based discharge and readmission rates but see much smaller reductions in the discharge-based readmission rate. In a companion blog to this piece, Joanne Lynn presents evidence that this attenuation of changes in discharge-based rates has happened repeatedly in community-based readmissions programs. We do not know, at this point, whether attenuation of changes translate into financial penalties but it seems very likely to increase a hospital’s risk.
We also do yet fully understand what specific changes produce these decreases in the population-based discharge rate, but the most parsimonious explanation is that the causes are pretty much the causes of reduced readmissions: Provide urgent care with support for keeping the patient in the community, and you are likely to reduce all admissions, not just readmissions. Enroll more patients in medical homes, and the benefits will not disappear 30 days after hospital discharge. Improve nursing home communications with emergency rooms, and the benefits will not be limited to patients within 30 days after hospital discharge.
What we can foresee is that hospitals, already wary of readmissions reduction because it directly reduces revenue, will become doubly wary if they conclude that reducing discharges may also cause or increase the MRRP penalty. If CMS is penalizing hospitals and communities for succeeding at improving care and reducing costs, the reaction may threaten a very successful set of initiatives. The examples we report are for community-based efforts to reduce readmissions. Hospital-level calculations are generally beyond our capability. CMS can, however, easily determine whether, all else being equal, penalties are more likely or larger in areas where the population-based hospital discharge rate is declining substantially than elsewhere. That information is urgently needed.
What to do.
The purpose of the MRRP is to reduce the burden of readmissions on Medicare beneficiaries and the Medicare trust funds, so the important indicator of progress is the number of readmissions, not the percentage of discharged patients that are readmitted.
Healthcare quality measurement needs to catch up with the National Quality Strategy and add measures of the impact of care on the health of the population that will complement measures of the quality of individual episodes of care such as hospitalizations. In the case of readmission measurement for the MRRP, this need is substantially more urgent because there is good reason to fear that a hospital that engages with its community and does exactly what the MRRP hopes for is more liable to financial penalties under the current, discharge-based measure than it would be under a population-based measure.
The first step is to assess the degree of urgency by examining national evidence on actual penalties. If unreasonable penalties are at all frequent then the problem is far more urgent. This will be complex, because Epstein has already shown in cross-sectional studies that population-based hospitalization rates and readmission rates are positively correlated.[2] At the same time it will be important to develop population-based measures of readmissions and compare their impact on penalties with the impact of discharge-based measures. The obstacles are bureaucratic, technical, and political.
Bureaucratically, the most important obstacle has been a widespread belief that the Patient Protection and Affordable Care Act requires calculating discharge-based rates. In fact, the Act says only that penalties are to be determined from the ratio of observed to expected numbers of readmissions and is silent on how the expected number is to be calculated. The other bureaucratic problem is less tractable: Under current procedures, the steps laid out for implementing a new measure, both at CMS and at the National Quality Forum (NQF) would likely take several years. The process should be expedited if the analysis of current penalties indicates that hospitals are being penalized for success in reducing admissions.
The technical challenges of creating a population-based readmission measure for hospitals are substantial. First, the procedure must find a way to measure each hospital’s population-based hospitalization rate. Second, a method of risk adjustment must be developed and applied so that population-based readmission rates for each hospital and community can be compared. Although these methods are still evolving, adjustments for factors such as neighborhood deprivation[3] are actually easier at the population level. These are difficult tasks, but a first step good enough to improve on the existing model should be possible within a year.
Politically, hospitals will be concerned about accountability for the community hospitalization rate. They will recognize that if hospitals in areas with low hospitalization rates are protected, then hospitals in areas with high hospitalization rates will be more vulnerable.
Some have hoped that traditional risk adjustment could solve this problem, because the most likely scenario is that average risk of readmission increases as the number of discharges decreases. That prospect is not promising, because the most assiduous work on risk adjustment has produced tools of only moderate power. The prospects for solving this problem with improved risk adjustment are not promising.[4],[5]
When you find yourself in a hole you should stop digging. It seems prudent for NQF to suspend endorsement of the pending discharge-based readmission measures and for CMS to delay implementing discharge-based measures if NQF endorses them until CMS has studied and reported the extent to which readmission penalties punish hospitals that are actually reducing both admissions and readmissions and has laid out an approach to any problems found. Finally, the problem identified here underlines the importance of placing a population-based foundation under at least some measures of health care system performance.
Footnotes:
[1] Centers for Medicare and Medicaid Services. Readmission reduction program. Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html
[2] Epstein, A. M., Jha, A. K., & Orav, J. E. (2011 December 15). The relationship between hospital admission rates and rehospitalizations. New England Journal of Medicine 365(24).
[3] Kind, A. J. H., Jencks, S., Brock, J., Yu, M., Bartels, C., Ehlenbach, W., & Smith, M. (2014 December 2). Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Annals of Internal Medicine 161(11) 765-775.
[4] Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. (2014, July). 2014 measure updates and specifications: Hospital-wide all-cause unplanned readmission – version 3.0. Retrieved from https://altarum.org/sites/default/files/uploaded-publication-files/Rdmsn_Msr_Updts_HWR_0714_0.pdf.
[5] Kansagara, D., Englander, H., Salanitro, A., Kagen, D., Theobald, C., Freeman, M., & Kripalani, S. (2011 October 19). Risk prediction models for hospital readmission: A systematic review. Journal of the American Medical Association 306(15) 1688-1698.