1.5 How could a community system find and offer MediCaring to frail elderly people who would benefit?
This question requires attention to the specifics of how to define the population in a way that is practical, which ultimately requires working with the data that is actually available as communities start to implement MediCaring. The leading research definition of frailty is this: “A clinical syndrome in which three or more of the following criteria were present: unintentional weight loss (ten pounds in past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity.”[21] An elderly person with none of the indicators is “robust,” a person with one or two indicators is classified as “pre-frail,” and a person with three or more indicators is “frail.” This research definition is a welcome guidepost, but most of these elements are not in existing records, and a workable plan cannot require outreach in person to every older person to test the criteria for entry.
Furthermore, the MediCaring services should reach some elderly people who have not lost weight, strength or energy but who are already disabled from a major chronic condition or from a combination of multiple chronic conditions. Our definition of frailty includes disabilities and memory problems, so the scope is broader than the research definition. For example, a person living with the effects of a disabling stroke or moderate dementia might well have none of the research criteria, but the person would still be appropriate for a MediCaring Community initiative.
Once MediCaring becomes popular and well-known, people who are not yet frail, but who are quite old and realize that their next health challenge is likely to leave them more disabled and frail, might well want to be able to rely upon a care system that makes sense. This would parallel the commonplace practice of a woman who is hoping to become pregnant who establishes a relationship with an obstetrician-gynecologist ahead of time. In our frail elder population, a person at 90 years of age who realizes that her strength is declining and that her chronic emphysema is likely to pose complications during the coming winter might well want to join a coherent and sensible service delivery system tailored to her needs, even before actually becoming disabled.
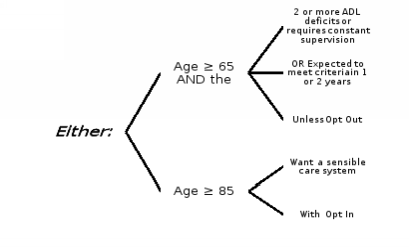
To help establish some practical approaches, we undertook analyses of Medicare payments and data from the Health and Retirement Study, which interviews a nationally representative sample of people older than 55 and their principal personal representative, every two years.[22] We tried out a criterion of having reported that the elderly person needed someone’s help with two or more of the six activities of daily living (ADLs) that are commonly catalogued. We set the bar at two ADLs because that is usually the level that requires nearly constant attendance by another person who is able to help, and because that is a common criterion for state Medicaid programs to cover a nursing home level of care. About one-tenth of all those over age 65 reported this level of disability in any one interview cycle, and only about one-tenth of them ever reported an improved level of disability before dying. This criterion fits common sense and either is or readily could be available, even by over-the-phone interview. A few people have this sort of disability only transiently, as when they are recovering from surgery, and that could readily be determined. The cohort could also include elders who have sufficient dementia to have poor judgment and require nearly constant attendance by another person, while still being able to do ADLs independently. As mentioned above, making MediCaring available to elderly people who are not yet disabled is justified when that person wants a sensible care system and is at increasingly high risks from age and lack of reserves when any additional health problems arise. In sum, the inclusion criteria could be as follows.
Figure 1.3: Identification of Frail Elders in Need of MediCaring
Of course, any particular community may have other data to use or priorities that justify different thresholds, so the first MediCaring Communities will need to adapt this initial set of criteria. In general, MediCaring Communities could start with people identified as they seek help in the medical care system. Most frail people now are in the hospital or the emergency room within any given year, so mining those records will yield the first set of potential MediCaring participants. One might be able to use the data gathered on admission to a nursing home (the Minimum Data Set [MDS] ) or a home care agency (the Outcome and Assessment Information Set [OASIS] data) to find people needing help with two or more ADLs. The Welcome to Medicare exam and the Annual Wellness Visit are Medicare preventive care planning visits that are being more broadly implemented and could serve to find frail elders within physician practices. In many parts of the country, Meals on Wheels and similar nutrition programs require nearly this level of disability, so implementing outreach through senior nutrition, programs will identify another cohort. As the program spreads and stories appear in local news media and in community settings like churches and clubs, referrals from family, elderly people, and their neighbors will arise. The aim would be to make MediCaring available to all who prefer the MediCaring approach and are eligible within a defined geographic area. Until all areas have a MediCaring program, there will be calls to serve some in a fringe around the local geographic boundaries, and communities will have to decide whether and under what conditions to allow a somewhat variable border.
For a frail elderly person, initiating MediCaring services should be available at any time. The 72 year old person with a profound stroke or the 92 year old who has just witnessed a difficult course for a similarly aged neighbor are in the sort of situation that motivates signing up for MediCaring. They need to be able to join when motivated and when their condition qualifies them to do so, without waiting for the Medicare annual enrollment period or even until the start of the next month.
In the early years, before the MediCaring program has a strong track record and experience with outreach and retention, respect for the participants requires that they be able to leave and return to traditional Medicare or perhaps to their previous managed care plan at nearly any time. Once the MediCaring Community program is well established, the administrative burden of allowing quick shifts might prove to be unnecessary.
[21] (Fried, et al. 2001)
[22] (Health and Retirement Study 2016)
