Core Component #1: Frail Elders Identified in a Geographic Community
The first key element of the MediCaring Communities service delivery reform is to develop a focus on frail elders—to recognize this newly common phase of life and to see that it has characteristic joys and troubles and also requires different social arrangements than those that served us earlier in life, even different from earlier in retirement age.
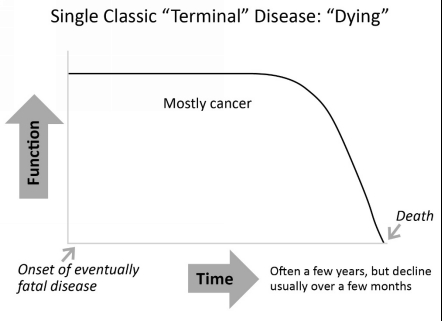
This sounds so straightforward, but that awareness is difficult to achieve, because simply acknowledging this phase of life is so new for our culture. Our cultural myth is that people live mostly healthy until they either die suddenly or contract a “serious” illness which turns into a “terminal” illness, following a course like Figure 1.1.
Figure 1.1: Classic “Terminal” Disease: “Dying”
However, now most of us will have a “frailty” course, much more like Figure 1.2, in which there is no clear “terminal” phase and the “dying” can be cut short by, for example, a pneumonia or a stroke, or the person can continue for remarkable lengths of time with increasingly severe limitations.
Figure 1.2: Prolonged Dwindling
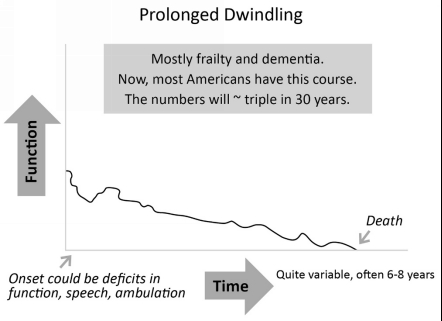
We have no popular stories about living through this part of life—no heroes, no villains, simply nothing useful. Elderly people searching for a reference point sometimes voice a strong preference not to live in a permanently unconscious status like the court cases of Ms. Theresa Shiavo or Ms. Karen Ann Quinlan, though the elderly person has no real likelihood of experiencing that outcome. Very few stories are well enough known to use as a benchmark. We know almost nothing of Ronald Reagan with dementia and what he and his caregivers went through. We have almost no movies or TV dramas (or comedies!) about this part of life. So, we have the remarkable opportunity, and the obligation, to create our myths and standards anew, and to be thoughtful about the stories we teach our children to admire. Indeed, once we recognize this nearly new phase of life, we can define its meaning in our lives. But the fact that the society has not yet built our stories and myths makes it difficult for people to identify the frail phase of life or to realize that it is very different to feel the limitations of chronic conditions in old age than to be ill when younger.
The language to use in dealing with policy and practice concerning frail elders deserves brief mention, and the reader will find a useful Glossary in the back of the book. This book will mostly use the term frail elders to refer to elderly people living with fragile health due to multiple chronic conditions and progressive disabilities. Some common terms tend to diminish the richness and humanity of frail elders. For example, elders are only patients or clients when in certain relationships. This category of frail elders includes elderly persons affected by serious illnesses or disabilities, including old age itself, that tend to worsen over time, greatly diminish resilience to stress, and require ongoing help from other people. This chapter will provide more details about defining the category.
Various professionals such as nurse practitioners and physician assistants have medical duties that overlap the role of the physician, but for simplicity, we will call them all physicians. Likewise, we will use family to include all those who are emotionally bonded to the frail elderly person, whether by friendship, relationship, or law, so family caregiver includes the long-term friend who provides personal care and coordination, just as a relative might. The diversity of our society requires that social policies be very inclusive and supportive of all who would help frail elders. LTSS stands for Long-Term Services and Supports. LTSS includes all the non-medical elements that go into supporting a frail elder across time, such as assistance with bathing and dressing and help buying and preparing food.
Finally, frail elderly people and their families have noticed that this is the last phase of life, and that the outcome is death, and they usually want to have this weigh in the decision-making and to be acknowledged. But our culture has only the language of “end of life,” “terminal disease,” and “ready for hospice.” These phrases do not usefully describe persons with persistently uncertain timing of death. So, we will work with longer phrases and helpful honesty, and the reader can try out language and phrasing that is supportive, kind, and honest.
This chapter responds to these key questions:
1. Who is frail and what characterizes that experience?
2. How do people transition into frailty?
3. Why organize services for frail people by geographic community?
4. Why refer frail elders to a MediCaring service delivery system?
5. How could a community system find and offer MediCaring to frail elderly people?
This is the online edition of MediCaring Communities
MediCaring Communities: Getting What We Want and Need in Frail Old Age at an Affordable Cost
List Price $9.95 at Amazon.com
Published June, 2016
194 pages, 6″ x 9″ (15.24 x 22.86 cm)
ISBN-10: 1481266918
Click cover for Amazon.com
