Core Component #4: Integrating Social and Supportive Services
For the last fifty years in the United States, medical care for elders has been enjoying very nearly a blank check from Medicare, with few effective constraints on utilization and a general cultural attitude that supports “leaving no stone unturned” by pursuing even long odds of benefit from medical services. On the other hand, supportive services for elders have been provided erratically, mostly as safety net programs, with little evaluation and many widely ignored gaps.
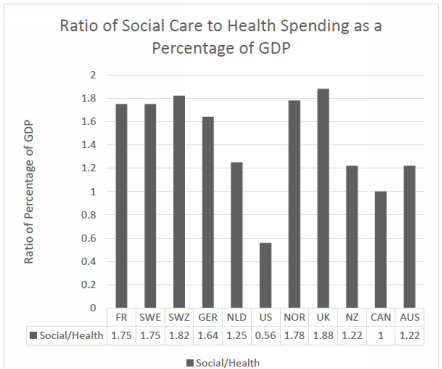
Bradley and Taylor showed that the U.S. spends about the same proportion of GDP on the combination of medical, social, and supportive services as most developed countries, but the U.S. uniquely spends much more on medical care (nearly double) and much less on social and supportive services (about half).[106] Figures 4.1 and 4.2 show the ratio of health spending to social service spending for several major countries.
Figure 4.1: Health Service and Social Service Spending (% of GDP)[107]
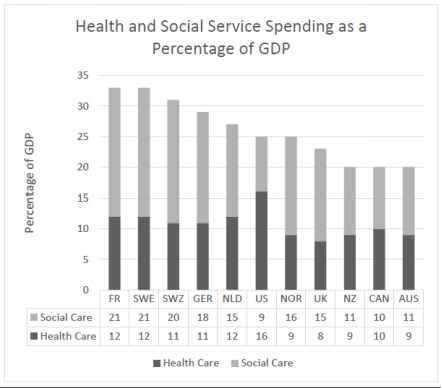
Figure 4.2: Ratio of Social to Health Service Spending (% of GDP)
In other countries, the services and budget for frail elders is a subject of political action, so a topic likehousing adaptation is in the public debate about priorities, alongside considerations of the desirability of more specialist physicians or another MRI machine. In the U.S., the delivery system provides no time and place at which the management functions for medical and social services come together, not even in local or state politics. At the federal level, these issues are in different agencies, different funding streams, and even different Congressional committees. These worlds have separate conferences, research methods and literature, funding streams, legislative committees, personnel training and incentives, and even different words used in the work. For example, medical providers call frail elders “patients,” while the social services world calls them “clients,” and in nursing homes, they are “residents.”
The elderly person and family often assume that some thoughtful folks have put together a care system that makes sense, but that is not the case. These services have grown up in response to needs and opportunities, with no substantial coordination or planning. In most other countries, eldercare issues come together in a socially sanctioned process: e.g., the county council in Sweden, or the Local Health Integrated Networks in Ontario, Canada.[108],[109] But not in the U.S.; we have no locus at which responsibilities for the needs of the frail elderly population come together, or for anyone to set priorities and monitor progress. But for frail elders to thrive, these domains of services must interact and collaborate, and priorities among them need to be set in order to serve the interests of the population. This does not now happen; medical care is so dominant and all other services are so stunted that overuse of medical services is rife and shortcomings in supportive services abound.
This overspending on medical care, slim availability of social and supportive services, and lack of anyone seeing the whole picture or taking responsibility for addressing critical needs yields a bizarre truth: In the U.S., a physician can write a prescription for a very expensive medication that is not likely to work for an elderly patient; but that physician cannot get home-delivered meals for this patient, nor can anyone else. In some parts of the country, waiting lists for Meals on Wheels exceed 4,000 people.[110] Indeed, in my travels I’ve found cities where the wait is sometimes a year long. Thomas and Mor estimated that increasing support for home-delivered meals by 1% would save 1,722 Medicaid beneficiaries from placement in a nursing home.[111]
These striking waiting times are allowed to grow despite the obvious suffering and malnutrition of frail elders and the evidence showing that home-delivered meals can help prevent frail elders from entering nursing homes.[112] On the other hand, Medicare coverage does not generate any wait for a high-cost, low yield drug, test, or treatment. A MediCaring Community can address this distortion by assessing all needs and shifting some resources to address the critical shortcomings of their local system. Efficiency demands that responsibility for particular services be matched with expertise; for example, housing experts should be working on housing, rather than leaving it to physicians and hospital social workers whose only easily accessed option ordinarily is nursing home placement.
The hallmark of frailty in old age is an increasing dependency on others. Medical services are important, of course, but the basics of living often become the elderly person’s main concerns: food, clothing, shelter, basic hygiene, socialization and meaningfulness, burdens imposed upon family caregivers, and impoverishment from the costs of purchased services. The well-funded medical care system has been largely blind to these issues, assuming that “someone else” is responsible, but being paid well to pick up the pieces when inadequate attention to these needs generates a medical crisis. The nation did acknowledge the role of long-term supports in passing the Older Americans Act as part of the trio that shaped Medicare and Medicaid fifty years ago.[113] However, the Older Americans Act has been ignored and underfunded and the U.S. has not really confronted or resolved the challenges posed by ever larger numbers of persons needing a great deal of help in order to live reasonably well in old age.[114] Instead, we’ve enabled medical care to provide rescue when things get very bad. The time has come for a more balanced approach that would supplement and monitor social and supportive services, aiming to learn how to provide the optimal array of services to ensure that frail elders can live as comfortably and meaningfully as possible, at an affordable cost to them, their families, and the society at large.
This chapter responds to these key questions:
4.1 What are long-term services and supports (LTSS)?
4.2 What are the roles of family caregivers and direct care workers?
4.3 How is eldercare financed now?
4.5 How will a MediCaring Community integrate LTSS and medical services for the local system?
[106] (Bradley and Taylor 2013, pp. 4-14) The OECD and the authors define health service expenditures as public and private spending on curative care, rehabilitative care, long-term care (not including personal care and ADL assistance), ancillary services such as diagnostic imaging, lab tests and patient transport, outpatient medical goods, prevention and public health services, health administration, and health insurance and healthcare capital expenditures. Social services expenditures include public and private spending on old-age pension and support services for older adults, survivors benefits, disability and sickness cash benefits, family supports, employment programs such as public employment services and employment training, unemployment benefits, supportive housing and rent subsidies, and other social services that exclude health expenditures.
[107] Figures 4.1 and 4.2 are based on data in Bradley and Taylor 2013, pp. 15 and 17. “GDP” refers to Gross Domestic Product.
[108] (Ontario Local Health Integration Network n.d.)
[109] (Government Offices of Sweden n.d.)
[110] Personal communication from Erika Kelly, Chief Advocacy and Government Affairs Officer, Meals on Wheels America, May 18, 2016.
[111] (Thomas and Mor, The Relationship between Older Americans Act Title III State Expenditures and Prevalence of Low-Care Nursing Home Residents 2013)
[112] (Thomas and Mor, Providing More Home-Delivered Meals Is One Way To Keep Older Adults With Low Care Needs Out Of Nursing Homes 2013)
[113] (Older Americans Act of 1965, Public Law 89–73 1965)
[114] (Parikh, Montgomery and Lynn 2015)
